New ONC-Sponsored Research Advances Health Information Exchange
Health information exchange (HIE) is not easy. ONC has sponsored expert research on various technical and business-related health information exchange topics, because we know that professionals engaged in implementing health information exchange must possess business acumen and technical expertise, on top of policy savvy and many other competencies. Without these skills there are many ways to overreach, or just as perilously, under reach, resulting in failure to maximize the long-term value of services offered through health information exchange.
The ONC-sponsored research will provide health information exchange implementers, policymakers, and researchers with a heightened understanding of several high-impact services that can support the sustainability of health information exchange organizations.
We would like to announce that five new health information exchange research reports are now available on HealthIT.gov. Each provides:
- Background information on core concepts
- Analyses of key challenges and opportunities
- Rich appendices, including up-to-date case studies
- Health information exchange vendor descriptions
To execute this work, ONC contracted with Audacious Inquiry  , a health information technology services company. These reports will support the State HIE Program’s grantees as they continue to implement health information exchange, which increasingly includes launching query-based exchanges.
, a health information technology services company. These reports will support the State HIE Program’s grantees as they continue to implement health information exchange, which increasingly includes launching query-based exchanges.
Listed below are the five new HIE reports that are available:
1. REPORT: Query-based Exchange: Key factors influencing success & failure of health information exchange
Perhaps the broadest of the reports, Query-Based Exchange: Key Factors Influencing Success and Failure provides essentially a “how-to” guide for navigating the major business considerations facing an HIE, including a breakdown of what the authors consider to be the determinants of HIE success. These are:
- Data provider distribution
- Data diversity/data saturation
- Breadth/relevance of the user-base
- Utilization rates
The report states that:
“…arriving at the true tipping point for query services that will make a Health Information Organization a clinical necessity is dependent on reaching certain milestones against [these] four interrelated metrics.”
REPORT FINDING: The Number of Patient Record Queries Indicate Success of HIEs
One of the most revealing aspects of this report is a chart contrasting six successful HIEs with two shuttered organizations across nearly 24 data points. One of these data points is the average number of patient record queries per month that each entity is receiving or had received. Those HIEs that are considered successful have figures ranging from 1,548 to 333,333 per month, while the closed HIEs had between 167 and 250 queries per month.
REPORT FINDING: There are Leadership Challenges for Health Information Exchange Vendors
The report also considers specific lessons from the experience of these health information organizations. It details the challenges of hiring and retaining a chief executive who is responsible for strategic vision, sales, marketing, day-to-day operations, and complex technical implementation projects. The research found that on top of all this, the leader might only receive a modest salary relative to her private sector counterparts.
2. REPORT: Health Information Exchange-Driven Notification & Subscription Services.
While health information exchange is not easy, it need not be overly complex. One theme that runs throughout the research is that basic tools can be used to support sophisticated use cases.
The report on HIE-Driven Notification & Subscription Services provides a review of the technical considerations involved in enabling push messages to providers. While these messages are a relatively simple technology, they can be used to support the advanced care coordination requirements of new payment models such as the Centers for Medicare & Medicaid Services’ Accountable Care Organizations. The report uses, as an example, the Indiana Health Information Exchange (IHIE)’s ability to send hospital admission alerts and discharge summaries to primary care providers. Such tools will be essential as hospitals begin to face negative financial incentives for readmissions, such as through CMS’ Readmissions Reduction Program.
The report also touches on how IHIE is developing a pilot that will allow managed care organization case managers, as part of their care coordination efforts, to receive notifications when their members are admitted to a hospital or visit an emergency department.
3. REPORT: Provider Directory Solutions for Health Information Exchanges and Beyond
Another important aspect of health information exchange is provider directories. While they are not glamorous, they are ubiquitous, and they can be highly valuable. On the most basic level, a provider directory is a type of electronic white pages that allows one provider to look up contact information for another provider.
The report on Provider Directory Solutions covers the key concepts associated with the technology. However, it also describes several additional use cases, such as how they can be used for future health benefits exchanges or for state licensing boards. Yet, the report goes even further by supporting the idea that the profit potential of provider directories is likely to go beyond the fundamental requirements of clinical health information exchange. Such considerations are critical for the State HIE Program’s cooperative agreement partners as they seek strategies to attain sustainability beyond the grant period.
4. REPORT: Master Data Management within Health Information Exchange Infrastructures
The report on Master Data Management within HIE Infrastructures explores the technical aspects of the tools that can help HIEs accurately capture and coordinate a patient’s identity. In short, master data management is how two pieces of electronic health information are appropriately merged or kept separate, which is particularly challenging when there are varying levels of data quality on patient identities.
The report also considers how master data management tools can be employed for advanced uses, such as data analytics associated with new payment models or patient centered medical homes.
5. REPORT: Consumer Engagement in Health Information Exchange
The report, Consumer Engagement in Health Information Exchange, provides a solid primer on the challenges and technical aspects of consumer-mediated exchange. This includes the considerations related to identity proofing, identity authentication, and access. The report also presents short case studies on several well-known entities working in this space, including:
For More Information
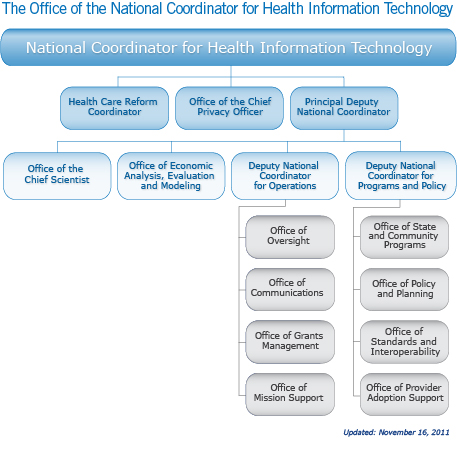
This work was overseen by the State HIE Policy Office, which is part of the State HIE Cooperative Agreement Program. ONC plans to release additional reports in the future.
For more information, contact ONC Program Analyst John Rancourt or ONC Program Manager Lee Stevens.