Revised Health IT Strategic Framework Presentation:
HIT Policy Committee Strategic Plan Workgroup
Meeting May 11, 2010, ”the purpose of today’s session (of the HIT Policy Committee Strategic Plan Workgroup) is to:
• Review specific changes made to the Strategic Framework
–Public listening session input
–Mapping of objectives and strategies
• Review and finalize the revised Health IT Strategic Framework for recommendation to HITPC on May 21, (2010).
Meeting Materials
|
|
Meeting
Audio
|
|
Excerpts from the “Health IT Strategic Framework: Strategic Goals, Prinicples, Objectives, and Strategies,” Office of National Coordinator for Health IT, May 10, 2010, Version 41. PDF Version
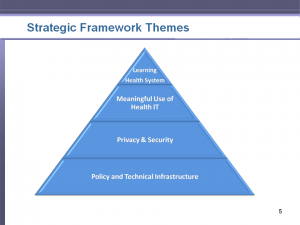
The Health IT Strategic Framework (the Framework) has four goals, which relate to the following areas:
Learning Health System
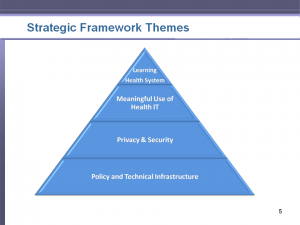
Strategic Plan Framework Themes
Meaningful Use of Health Information Technology
Privacy and Security
Policy and Technical Infrastructure
STRATEGIC FRAMEWORK SCOPE and APPROACH
The HIT Policy Committee Strategic Plan Workgroup was chartered to provide recommendations to the full committee on the Federal Health IT Strategic Plan development and provide the vehicle through which private and public input and coordination was achieved.
A. Health IT Strategic Framework Scope
The Health IT Strategic Framework encompasses three levels:
o The full array of entities in the public and private sectors who have a role in affecting and implementing the use of HIT to improve health and health care;
o The broad array of Federal HIT policies, regulations, systems, and activities; and
o The specific mandate, authorities, and role of the ONC.
The Framework emphasizes the implementation of legislative imperatives to achieve widespread adoption and meaningful use of HIT.
The Framework also focuses on features that would be essential to continue the adoption and value of HIT beyond ARRA funding.
The Framework focuses on 2011 through 2015 time period and on laying the ground work for the period beyond 2015 to create a learning health system through the effective use of HIT.
B. Health IT Strategic Framework Approach
The process to develop the Framework was participatory with broad involvement across the health care sector with opportunities for public input and discussion.
The Framework was developed by the Workgroup, with input from other stakeholders, and includes recommendations regarding goals, principles, objectives, and strategies.
The Framework includes priorities and initiatives that are achievable.
This Framework provides guidance to ONC in the creation of the Federal Health IT Strategic Plan Update.
Vision
A learning health system is a system that is designed to generate and apply the best evidence for the collaborative health care choices of each patient and provider; to drive the process of new discovery as a natural outgrowth of patient care; and to ensure innovation, quality, safety, and value in health care. (Charter of the Institute of Medicine Roundtable on Value & Science-Driven Health Care).
A learning health system focuses on the needs of individuals and population health and aims to be patient-centered, safe, timely, effective, efficient, and equitable while protecting privacy and confidentiality of health information. In a learning health system, individuals can make informed decisions about their health and health care; patients can exercise informed choices about sharing their data; decision makers have access to the right information at the right time in a secure environment; the health delivery system is more efficient; and all participants in the system contribute to improving population health.
There are a number of activities that go on into this learning health system. Consumers are engaged, and processes are continuously improved and new innovations continue to improve the health status of the population. Education and research improves the knowledge base upon which services are delivered. The beneficiaries are numerous. If everything is working correctly, this information about the experience of care is manifested as data to produce the results. Therefore, patients are more informed and the quality of care is improved. This means improved outcomes for individuals, as well as the population. The value of the healthy system is enhanced, and new, shared knowledge is created.
Health information technology (HIT) provides a critical infrastructure for a learning health system and provides a platform for health reform goals related to quality improvement and payment reform. HIT offers tools (i.e., electronic health records, personal health records, mobile health and consumer e-health applications) that can expand current capabilities to collect and manage data that can help creation of a sustainable system that facilitates getting the right care to people when they need it and then captures the results for improvement in care, and create and share knowledge.
Despite the important role of HIT to a learning health system, only a small number of health care organizations have implemented a comprehensive EHR. Getting to widespread adoption and use of HIT is one component of a reformed system – necessary, but not sufficient, to effect the broad change needed in our health system. Transformation of our health care system will take three components working together – people, process and technology.
Inherent in the vision of a learning health system is a set of values that provide the foundation for public policies at the Federal and state levels aimed at reforming and improving the health system. The HITECH Act specifies this broader set of values and helps to focus Federal health policy regarding information technology in the following areas:
Improving privacy and security protections for health information;
Facilitating individual access to his or her health information;
Improving quality of health care by improving care coordination, reducing medical errors, reducing chronic disease, reducing health disparities, improving population health, and advancing research and education;
Addressing the needs of children and other vulnerable populations;
Collecting information for quality reporting, biosurveillance, public health, medical and clinical research, and drug safety; and
Improving efficiency and reducing the burden on patients and health care professionals.
The HIT policies and programs of ONC and its Federal partners aspire to achieve this vision and its inherent values, leveraging the programs authorized by the HITECH Act. To achieve this vision, a transformation of our current health care delivery system is required.
To begin this transformation, the Federal government proposed a set of priorities for meaningful use of HIT which can also be applied broadly to help achieve the vision. They include:
Improve quality, safety, efficiency and reduce health disparities;
Engage patients and families in their health care;
Improve care coordination;
Improve population and public health; and
Ensure adequate privacy and security protections for personal health information.
Implicit in implementing the HITECH Act and addressing these health priorities are a number of roles that only the Federal government can play in promoting the adoption and use of HIT. One key role involves the provision of resources to support the infrastructure that serves “public goods” including public health, biomedical research, quality improvement, and emergency preparedness. The government also has a role to play when information asymmetries hinder the development of a private market. The efforts involving standards, implementation specifications, and certification criteria are a solution to such problems. Government action is also necessary to spur the adoption of HIT and the development of means for health information exchange to assure the critical mass of users necessary to create a self-sustaining system of interoperable HIT. Finally, working to improve the efficiency of public and population health programs is clearly a government responsibility.
The Health IT Strategic Framework enumerates critical government roles in the pursuit of a health system that uses information to empower individuals and to improve the health of the population.
Background
In the development of the Strategic Framework, the Strategic Plan Workgroup deliberated on many key issues and challenges. The deliberations involved juggling many conflicting ideas such as the importance of addressing short-term needs in the face of longer-term uncertainties; finding the right balance between technology innovations, regulatory approaches, and other constraints and risks associated with use of information technology; and others.
As such, the Federal Health IT Strategic Plan should be a living document that adjusts to the changing health environment. Among the topics discussed during the development of this Framework were the following:
Transparency and Access – ensuring that patients have access to information and knowledge to make informed decisions about their care;
Personal Choice – finding the right balance between patient privacy and patient choice (i.e., some patients do not want their data shared whereas some patients do not mind sharing or want to share their information for research, improved care, and/or for the betterment of society);
Public Engagement – allowing for continued public discussion and debate on current and emerging health care issues that cannot be resolved easily or through easy technology solutions;
Technology Innovation – learning from the impact that the internet and social networking has had on our daily lives, and leaving flexibility for how technical innovations may change the delivery of health care; capitalizing on the promise of emerging new technologies while preserving the rights of individuals;
Support for Research – putting in place appropriate policies and technical infrastructure to allow researchers to access a spectrum of data to support new discoveries and treatments while protecting individual privacy; and
Unintended Consequences – allowing for processes to capture and learn from unanticipated adverse consequences of HIT use, and developing actions to mitigate and prevent untoward effects.
This Framework is intended to set an approach and priorities for moving forward, rather than identifying a complete set of actions that would facilitate widespread adoption and use of HIT. This Framework describes strategies and HIT infrastructure that can serve as a foundation for developing programs that enhance the quality of health care, population health, privacy and security protections, and other values inherent in the vision.
Excerpts from slide presentation for May 11, 2010 meeting of Health IT Policy Committee Strategic Plan Workgroup.
PPT version.
Policy and Technical Infrastrucure
What Do We Aim to Accomplish with Appropriate Policy and Technical Infrastructure?
–Establish policies, standards, and cetification criteria to incrementally enhance the interoperability of HIT.
–Facilitate the development of market-susatainable mechanisms to ensure reliable, secure exchange of health information.
How Do We Plan to Accomplish It?
–Identify and prioritize types of data for transmission that facilitate improvement in national health priorities
–Adopt standards, specifications and certification criteria that enhance interoperability, functionality, utility and security of HIT
–Enable secure exchange of health information over the Internet to support clinical care and population health
–Encourage development of innovative technology
–Engage public and private sector to explore mechanisms to increase business demand and public support for information exchange
–Expand broadband access to support health and health care –Establish certification and testing program of EHR technology
–Assess and address patient safety issues that may arise from HIT
Privacy and Security
What Do We Aim to Accomplish with Appropriate Privacy and Security Protections?
-Develop and enforce privacy protections for all aspects of information management
-Increase understanding, implementation of laws and policies that protect privacy of health information
-Improve accuracy of electronic health information through widespread consumer access
Meaningful Use of Health IT
What Do We Aim to Accomplish using HIT?
-Improve health and health care through meaningful use of HIT
-Leverage public- and private-sector resources and policies to accelerate adoption of HIT
-Engage patients and caregivers in shared healthcare decision making
-Improve efficiency and reduce administrative burden on providers and patients through HIT
How Do We Plan to Accomplish It?
–Develop meaningful use roadmap
–Train and support a knowledgeable HIT workforce
–Target HIT investments to address national high priority health issues
–Use national health priorities for which effective use of HIT has demonstrated impact to guide selection of future criteria for assessing the meaningful Use of HIT
–Actively support primary care and other small providers to achieve meaningful use of certified EHR technology
–Promote participation of all members of the health team
–Provide resources to facilitate achieving meaningful use for eligible providers and eligible hospitals
–Encourage health care professionals not eligible for meaningful use incentives to achieve meaningful use and improve health outcomes
–Facilitate development of HIT to support care communication and coordination among consumers and their health care professionals
–Provide the tools and assistance to providers and consumers that can address the key workflow and behavioral changes necessary for meaningful HIT use
–Develop a comprehensive communication strategy to engage consumers
–Promote increased usability through consumer-centered design in certified EHR technology and other HIT products
–Coordinate and leverage programs to advance the meaningful use of HIT with the administrative simplification requirements of Health Reform and the requirements for HIPAA transaction upgrades and the implementation and use of ICD-10
Learning Health System
What Do We AIm to Accomplish by Supporting a Learning Health System?
-Leverage networked HIT to facilitate creation of knowledge through consistent policies, standards, and methods
-Execute comprehensive education campiagn to promote shared vision of a learning health system enabled by HIT
-Leverage data from populations ot advance the understanding of health, disease, and treatments
How Do We Plan to Accomplish It?
–Engage public- and private-sector stakeholders to effectively leverage data and human resources
–Incorporate global health into the interoperability requirements
–Harmonize meaningful-use requirements with the needs of population health and a learning system
–Continuously evaluate successes and lessons learned from HIT adoption and incorporate best practices into HIT programs
–Support individuals’ informed decisions to allow use of their data for societal benefit
-Develop and implement tools to improve consumers’ health and HIT literacy to facilitate shared decision-making and promote self management and self efficacy
–Communicate with professional societies and boards to identify opportunities for meaningful use activities to contribute to professional education programs
–Reward and leverage industry best practices and uses of HIT to create a learning system that supports advances in health promotion and disease treatment, while making knowledge and technology more accessible.
–Stimulate and support innovations in care delivery, performance measurements, genomics, and comparative effectiveness through HIT
–Support research and development activities to overcome obstacles that impede creation of learning systems
If you have any technical questions, please send an email to webmeeting@altarum.org